Cerebral Cavernous Malformations
- Jan 14, 2025
- 4 min read
Updated: May 7, 2025
Dr. Prem Pillay , Singapore Brain Spine Nerves Center, Singapore
Senior Consultant Neurosurgeon with super speciality training in Neurosurgical Oncology
(Fellow at MD Anderson Cancer Center and Hospital, U of Texas, USA)

What Are Cerebral Cavernous Malformations?
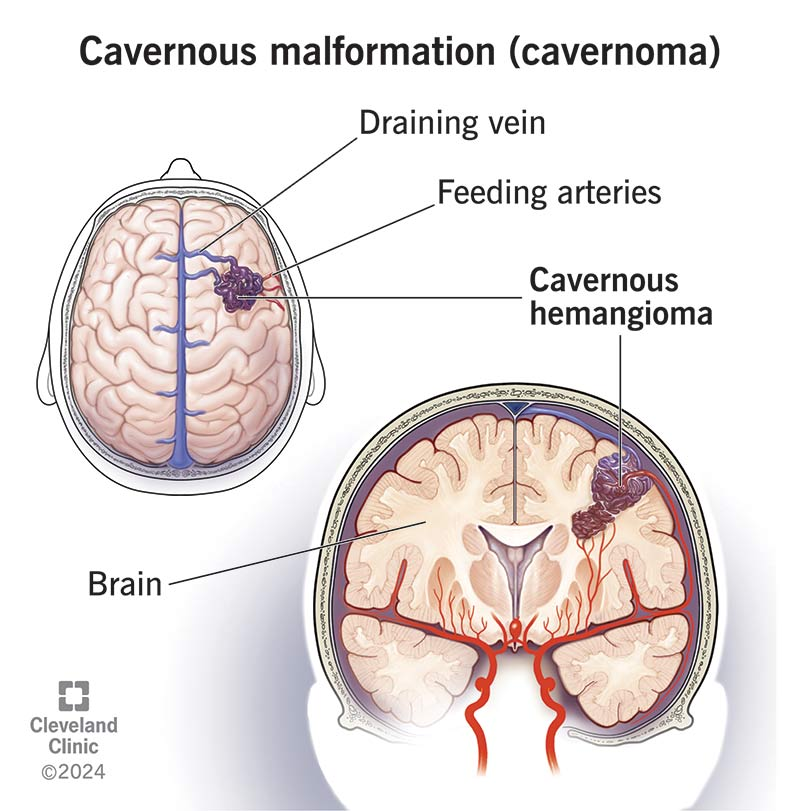
Cerebral cavernous malformations (CCMs), also known as cavernous hemangiomas, cavernous angiomas, or cavernomas, are abnormal clusters of blood vessels in the brain or spinal cord [1][3].Dr Prem Pillay explains that these lesions are characterised by their distinctive appearance, resembling small mulberries, and are composed of closely packed, thin-walled blood vessels [5].
CCMs contain slow-moving or clotted blood and lack the normal junctions with surrounding cells, leading to potential leakage into adjacent tissues [1].
Unlike tumours, CCMs do not exhibit endothelial hyperplasia and are considered vascular malformations rather than neoplasms [1]. These lesions can vary in size but are typically less than 1 centimetre in diameter [5].They can be found in various locations within the central nervous system, including the white matter of the brain, the cerebral cortex, and the spinal cord [1]
Causes and Genetic Factors
The aetiology of CCMs is complex and can be attributed to both sporadic occurrences and genetic factors.
In many cases, CCMs develop sporadically as single lesions without a clear hereditary component [5].
However, a significant proportion of cases are associated with specific genetic
mutations.
Genetic Basis of Cavernomas / CCMs
CCMs can be inherited in an autosomal dominant pattern, caused by mutations in three primary genes:
CCM1 (KRIT1)
CCM2 (MGC4607 or malcavernin)
CCM3 (PDCD10) [1]
These genes play crucial roles in maintaining the integrity of blood vessels.Mutations leading to loss of function in these genes are believed to be responsible for the formation of CCMs [1].
The “second hit mutation” theory suggests that a combination of inherited and acquired mutations may contribute to the development of multiple lesions in some patients [1].
Diagnosis of CCMs / Cavernomas
Accurate diagnosis of CCMs is essential for proper management and treatment planning.
Common diagnostic methods include:
Magnetic Resonance Imaging (MRI)
MRI is the gold standard for diagnosing CCMs.
On T2-weighted images, CCMs typically appear as high-signal lesions [1].
Gradient-echo or susceptibility-weighted sequences can enhance the detection of small or multiple lesions.
Computed Tomography (CT)
CT may show CCMs as areas of increased density, often with calcifications.
MRI is preferred due to superior soft tissue contrast and ability to detect smaller lesions [1].
Angiography
CCMs are angiographically occult and do not appear on conventional angiograms [3].
Cerebral angiograms are useful to distinguish CCMs from small arteriovenous malformations (AVMs) or concurrent AVMs/AV fistulas.
Genetic Testing
For patients with a family history or multiple lesions, genetic testing for CCM1, CCM2, and CCM3 can confirm diagnosis and guide management [3].
Treatment Options
The management of CCMs is tailored to each patient’s presentation, lesion location, and symptoms.As a Cavernoma expert, Dr Prem Pillay offers a comprehensive treatment approach using the latest advancements in neurosurgery and radiosurgery.
Conservative Management
For asymptomatic lesions or those in deep, eloquent brain areas, a watchful waiting approach may be appropriate.This includes:
Regular MRI monitoring to track growth or changes [6]
Lifestyle modification guidance and identifying potential triggers to reduce risk
Microsurgical Resection
Surgical removal is the definitive treatment for symptomatic CCMs, particularly those causing recurrent haemorrhages or intractable seizures [8].Dr Prem Pillay employs state-of-the-art techniques to maximise safety and efficacy:
Frameless stereotaxy for precise lesion localisation
Intraoperative functional MRI to map critical brain areas
Computer image-guided surgical navigation for optimal planning [7]
The goal is complete resection while preserving healthy tissue — shown to provide excellent outcomes in epilepsy control and haemorrhage prevention [8].
Stereotactic Radiosurgery (SRS)
For deep-seated lesions in eloquent areas or for patients unfit for surgery, SRS is a valuable alternative [8].
Uses highly focused radiation beams to target CCMs precisely
Reduces risk of future haemorrhages
Performed with Gamma Knife or LINAC Radiosurgery using robotic assistance
Day procedure: scarless, painless, and involves no cutting
Medical Management
While there is no medication to treat CCMs directly, symptom management includes:
Anticonvulsants for seizure control
Pain management for headaches
Steroids to reduce perilesional oedema when indicated [4]
Ongoing Research and Future Directions
As a Neurosurgeon with CCM expertise, Dr Prem Pillay actively follows cutting-edge research to improve outcomes. Current focus areas include:
Novel pharmacological agents targeting CCM signalling pathways
Advanced imaging techniques for better lesion characterisation
Minimally invasive surgical approaches for deep lesions
Conclusions
Cerebral cavernous malformations are complex vascular lesions that require expert management.With many years of experience and access to advanced technology, Dr Prem Pillay delivers the highest standard of care — from accurate diagnosis to tailored treatments.
If you or a loved one has been diagnosed with a CCM, we encourage you to consult with our specialised team.Together, we can create a comprehensive treatment strategy tailored to your unique needs and goals.
Citations
[1] https://en.wikipedia.org/wiki/Cavernous_hemangioma[2] https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/cavernous-malformations[3] https://www.ninds.nih.gov/health-information/disorders/cerebral-cavernous-malformations[4] https://www.healthline.com/health/cavernous-hemangioma[5] https://www.mayoclinic.org/diseases-conditions/cavernous-malformations/symptoms-causes/syc-20360941[6] https://my.clevelandclinic.org/health/diseases/21594-cavernous-hemangioma[7] https://www.mountsinai.org/locations/cerebrovascular-center/conditions/vascular-malformations/cavernomas[8] https://pmc.ncbi.nlm.nih.gov/articles/PMC4300037/[9] https://www.mayoclinic.org/diseases-conditions/cavernous-malformations/diagnosis-treatment/drc-20360942



