Medulloblastomas/Primitive Neuroectodermal Tumours (PNET)
- Jan 14, 2025
- 5 min read
Updated: May 6, 2025
Dr. Prem Pillay , Singapore Brain Spine Nerves Center, Singapore
Senior Consultant Neurosurgeon with super speciality training in Neurosurgical Oncology
(Fellow at MD Anderson Cancer Center and Hospital, U of Texas, USA)
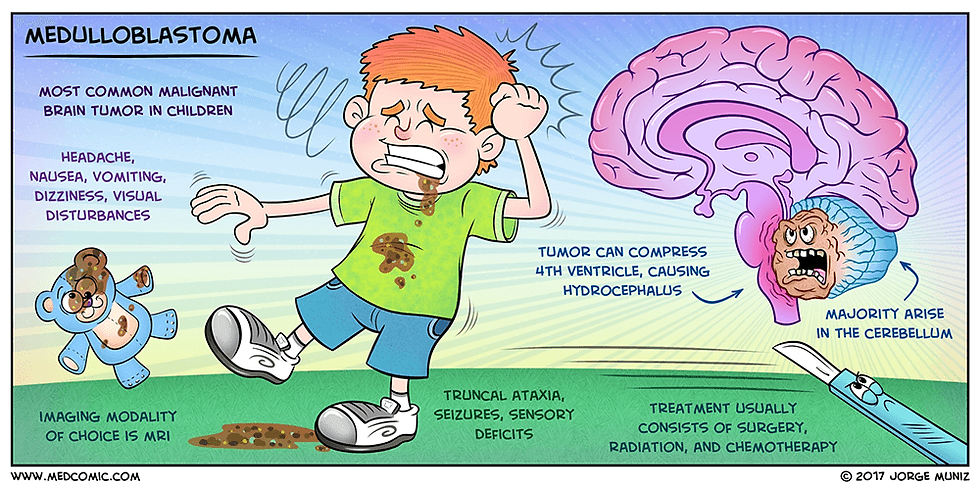
Medulloblastoma
Medulloblastoma (MB) is an embryonic tumor of the neuroepithelial tissue and the most frequent primary pediatric solid malignancy. MB represents a heterogeneous group of cerebellar tumors characterized clinically by increased intracranial pressure and cerebellar dysfunction, with the most common presenting symptoms being headache, vomiting, and ataxia.

Epidemiology
MB is the most common malignant brain tumor in childhood. Annual incidence is estimated at 1/909,000 in Europe, 1.5/100,00 in the USA said Dr Prem Pillay , a Neurosurgeon who specializes in treating Medulloblastomas ( He trained at the Cleveland Clinic,USA and the Hospital for Sick Children, Toronto). Males are more affected than females.
Clinic Description
Age of disease onset is variable and can occur in patients ranging in age from the newborn period to adulthood (peak age at presentation is children 3-6 years, with only 25% of patients being between 15 and 44 years). The most common presenting symptoms are headache, vomiting, and ataxia. Additional features that may be observed include lethargy, motor or cranial nerve impairment, gaze palsy, visual impairment due to hydrocephalia, vertigo/hearing loss, behavioral changes/irritability, and extracranial pain (e.g. back pain in those with spinal metastases). Around 30% of pediatric cases present with metastases at diagnosis. Most metastases occur within the central nervous system by seeding via the cerebrospinal fluid (cranial or spinal), while spread to extracranial organs (e.g. bone marrow, liver, lungs) is very rare at diagnosis. In a minority of patients, MB is associated with Gorlin syndrome, familial adenomatous polyposis (FAP; the association of FAP and MB is referred to as the Turcot syndrome with polyposis) or with Li-Fraumeni Syndrome (see these terms). Increased susceptibility to certain tumors (neuroblastoma), hematological malignancies (acute lymphoblastic leukemia, acute myeloid leukemia) or disorders caused by mutations in genes encoding components of the RAS signaling pathway (Noonan syndrome or neurofibromatosis-Noonan syndrome) have been reported in MB (see these terms).
Etiology and Molecular Genetics
To date, the exact etiology of MB is still unknown but genomic data has identified multiple candidate genes that contribute to the pathogenesis of different subgroups of MB. This includes an inhibitor of the sonic hedgehog pathway SUFU (10q24.32), the RNA helicase DDX3X (Xp11.3-p11.23), chromatin regulators KDM6A (Xp11.2) and N-CoR complex genes BCOR (Xp11.4), and the Parkinson’s disease genes KMT2D (12q13.12), SMARCA4 (19p13.3), MYCN (2p24.3), and TP53 (17p13.1).
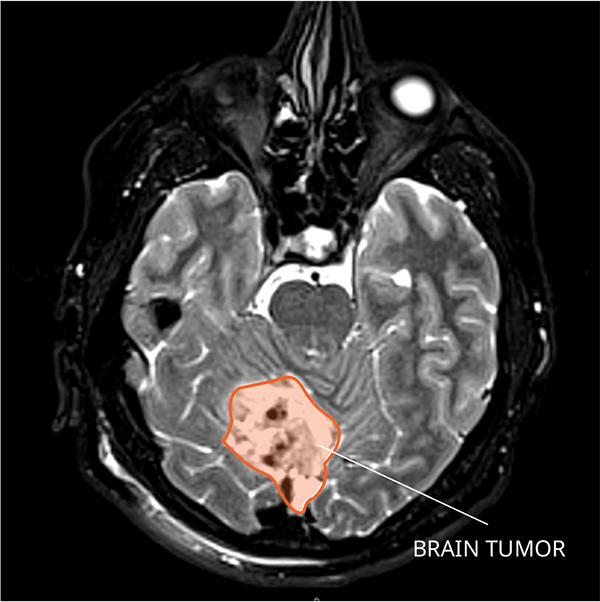
Diagnostic Methods

MB occurs in the vermis and 20% occurs in the hemispheres of the cerebellum. Histologically, MB is characterized by small, round cells that stain blue with haematoxylin spectrum and appearance ranges from tumors with extensive nodularity to those with large cell/anaplastic features. Apart from classical MB, four histological variants of MB are recognized: anaplastic MB, large cell MB, MB with extensive nodularity, and desmoplastic/nodular MB.
Differential diagnosis
Differential diagnosis includes other brain tumors (ependymoma, glial tumor, atypical teratoid rhabdoid tumor; see these terms) and other causes of cerebellar alterations (infectious or cystic lesions, hemorrhages).
Management and treatment
Initially, patients need to be checked for increased intracranial pressure.
The best current treatment is gross total resection of the Tumor using Microsurgery assisted with Computer aided Image guided technology, Ultrasonic tumor removal systems, Lasers, Microinstruments with Neuromonitoring particularly of brainstem signals followed by good ICU care stated Dr Prem Pillay who specializes in brain tumors including Medulloblastomas. The postoperative treatment depends on age, histological variant, and result of staging assessments. In children older than 3-5 years, craniospinal irradiation including Stereotactic Radiotherapy with MicroMLC technology can be applied. In younger children, brain sparing therapies avoiding irradiation can be administered in very specific constellations.
Latest Advances
Advances in Diagnosis :
Molecular Subgrouping
One of the most significant advances in medulloblastoma diagnosis has been the identification and characterization of molecular subgroups. Medulloblastomas are now classified into four main subgroups based on their molecular profiles:
WNT
SHH (Sonic Hedgehog)
Group 3
Group 4
This classification has important implications for prognosis and treatment planning. For example, WNT tumors generally have the best prognosis, while Group 3 tumors tend to have the worst outcomes.Improved Imaging Techniques
Improved Imaging Techniques
Researchers are developing new imaging methods to diagnose and monitor medulloblastomas more accurately. A recent study demonstrated that combining MRI scanning with machine learning could potentially identify medulloblastoma subtypes without the need for invasive biopsies.
This approach could significantly reduce diagnostic wait times from 3-4 weeks to just 10 minutes.Liquid Biopsies
Liquid Biopsies
Ongoing research is exploring the use of liquid biopsies (analyzing tumor DNA in cerebrospinal fluid, or blood ) to diagnose and monitor medulloblastomas non-invasively. This technique could provide real-time information about tumor genetics and treatment response.
Advances in Treatment :
Risk Adapted Therapy
Treatment protocols are increasingly tailored based on both clinical risk factors and molecular subgroup.
This approach allows for de-escalation of therapy in lower-risk patients to reduce long-term side effects, while maintaining or intensifying treatment for high-risk groups.
Reduced Radiation Therapy
For standard-risk patients, reducing craniospinal irradiation (CSI) from 36 Gy to 23.4 Gy, combined with oral and iv anti tumor agents , has shown similar survival outcomes with potentially fewer cognitive side effects.
However, further reduction to 18 Gy resulted in poorer outcomes, particularly for Group 4 tumors.
Proton Beam Therapy
The use of proton beam therapy for CSI and tumor bed boost is becoming more common. This technique can deliver precise radiation doses while sparing surrounding healthy tissue, potentially reducing long-term side effects.
Novel Chemotherapy Approaches
Recent studies have explored new chemotherapy regimens and timing:
The addition of a radiosensitizer showed improved outcomes for Group 3 patients in a post-hoc analysis of the ACNS0332 study
Neoadjuvant anti tumor agents before surgery is being investigated to potentially improve surgical outcomes and neuropsychological function
Immunotherapy
Several immunotherapy approaches are being studied for medulloblastoma:
Adoptive T-cell therapy combined with PD-1 inhibitors is being tested in a clinical trial for relapsed Group 4 medulloblastoma
An mRNA cancer vaccine is being developed to reprogram the immune system to attack medulloblastoma cells
Targeted Therapies
Researchers are identifying new molecular targets for medulloblastoma treatment:
An anti tumor agent originally developed for pancreatic cancer has shown promise in preclinical models of Group 3 medulloblastoma
Targeting specific regions of the EP300/CBP proteins, particularly the bromodomain, has demonstrated anti-tumor activity in Group 3 medulloblastoma cells
Infant Treatment Protocols
For infants (typically defined as under 4 years old), treatment approaches aim to delay or avoid radiation therapy due to its severe cognitive effects. Current strategies include:
High-dose anti tumor agents with stem cell rescue
Intrathecal and intravenous anti tumor agents
Combinations of these approaches
Future Directions
Further refinement of molecular subgrouping and identification of targetable mutations within subgroups.
Development of more effective and less toxic targeted therapies.
Optimization of immunotherapy approaches for medulloblastoma.
Improvement of treatment strategies for infants and young children to minimize long-term cognitive effects.
Integration of liquid biopsy techniques for real-time monitoring of treatment response and tumor evolution.
These advances in diagnosis and treatment offer hope for improved outcomes and quality of life for patients with medulloblastoma and other PNETs. However, continued research is needed to address the challenges posed by these aggressive pediatric brain tumors.
*The Hospital for Sick Children Toronto, Canada is one of the leading Pediatric and Childrens Cancer Centers in the world including for the treatment of Pediatric Brain Tumors. MD Anderson is one of the leading Cancer Centers in the USA and Globally.
Conclusion
Medulloblastoma and PNET are challenging tumours that require prompt and expert care. Early diagnosis and a multidisciplinary treatment approach are essential for improving outcomes and quality of life. If you or a loved one experiences persistent neurological symptoms seek immediate evaluation. Visit the Singapore Brain Spine Nerves Center for specialised care and support.



