Pituitary Tumours
- Jan 14, 2025
- 4 min read
Updated: May 9, 2025
Dr. Prem Pillay, Singapore
Senior Consultant Neurosurgeon with super specialty training in Neurosurgical Oncology
(Fellow at MD Anderson Cancer Center and Hospital, U of Texas, USA)
Pituitary tumors that occur from the pituitary gland which can be described as the “Master” hormone gland of the body which is located below the base of the brain and in front of the brainstem . It sits in a bony fossa (depression) called the sellar turcica. It is divided into an anterior lobe and a posterior lobe (with a small intermediate lobe).
Pituitary tumors account for about 15% of all intracranial tumors.
Mean age: 20 to 50 years
Sex: More females and males for prolactin and ACTH secreting tumors and a male predominance for GH-producing tumors.
Microadenomas are tumors less than 10 mm in size, and Macroadenomas are more than 10 mm in size. Local invasion can occur with macroadenomas, particularly into the skull base regions such as the cavernous sinus. Superior growth of macroadenomas can compress the optic chiasm/optic nerves and cause visual disturbances. Malignancy is rare (<1% of all pituitary tumors).
Prolactin producing tumors are the most frequent type of pituitary tumor (30%). Failure of menstruation (amenorrhea) and milk production from the breasts in non-pregnant females (galactorrhea) are the common symptoms. In men, decreased libido and impotence and visual loss are commoner symptoms, as the tumors tend to be larger when discovered.
GH secreting tumors are the second commonest hormone-producing pituitary tumors (15%).It can cause children to grow into “giants” (gigantism) and break height records in their communities. In adults, it can cause acromegaly with an enlarged head, hands, and feet.
ACTH producing tumors (10%) can cause Cushing’s disease. Such patients have central obesity, a moonface, and abdominal marks called striae.
TSH secreting tumors are rare (1%) and cause symptoms of hyperthyroidism.Null cell tumors are the second most common tumor and do not produce hormones (25%). They can grow to a large size and cause visual loss before detection. They can be invasive.
Diagnosis of Pituitary Tumours
This is based on the clinical symptoms and signs mentioned above. An emergency situation can be created by sudden bleeding in a tumor, called pituitary apoplexy. This can cause sudden loss of vision and even collapse and coma.
Blood tests of all the common pituitary hormones are carried out.
Vision tests such as Visual Fields and retinal photographs can reveal visual loss and its extent.
MRI with contrast (gadolinium) is superior to CT scanning in diagnosis, particularly for the smaller microadenomas. Some patients with ACTH producing microadenomas are difficult to find, and selective venous sampling of the hormone may be required by angiography.
Differential Diagnosis
Nelson’s syndrome is an enlargement of the pituitary gland caused by a surgical adrenalectomy.
Lymphocytic hypophysitis can cause a tumor-like appearance but it is an autoimmune disease.
Giant cell pituitary granulomas and Tuberculous granulomas can be mistaken for pituitary tumors on MRI or CT.
Treatment
Pituitary Tumors
Hormone-secreting tumors which are microadenomas can be treated by oral agents.
For tumors that do not respond to medical treatment or if patients have side effects from medical treatment, then alternatives are surgery or radiosurgery.
Surgery
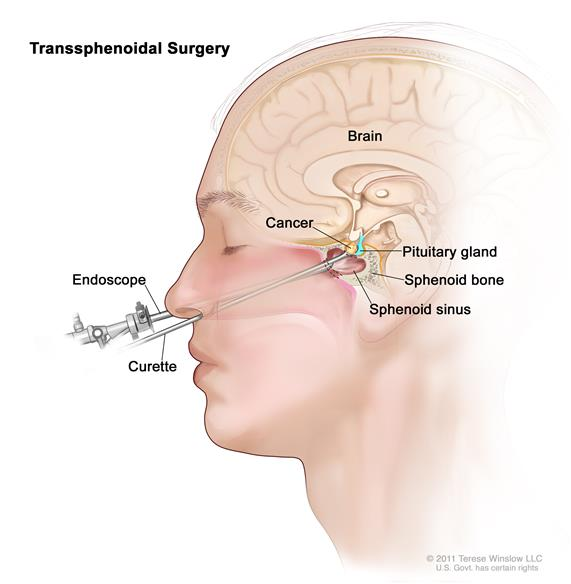
In the past, this was carried out using an open craniotomy, and then later with open approaches through the nose or above the teeth through the mouth.
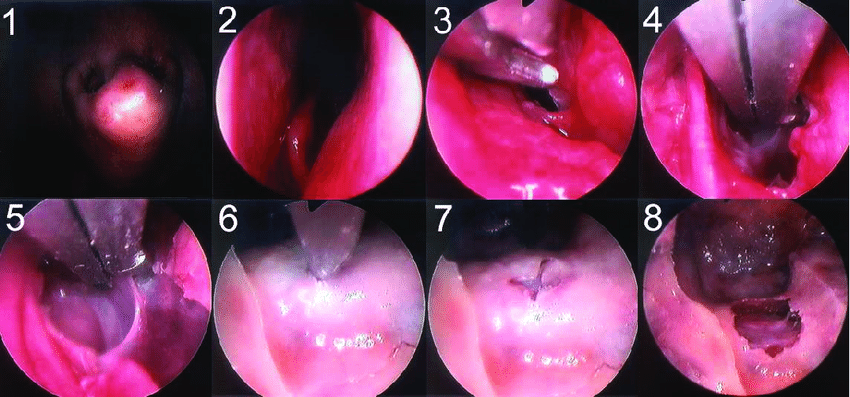
Modern approaches include Endoscopic approaches through the nasal passages with microsurgical methods.
Computer guidance (StealthStation) can be used to guide such minimally invasive microsurgery.
Radiosurgery
Gamma Knife and stereotactic radiotherapy (SRT) are more focused treatments than traditional radiotherapy. There is a more precise treatment of tumors with fewer side effects.
The latest technologies include:
Tomotherapy (NeuroTomotherapy)
MicroRadiosurgery (using a robotic couch and the latest fine MMLC)
Proton Therapy systems
Combined Endoscopy/Microsurgery and Radiosurgery
In patients with large invasive tumors, combination treatment may be safer and more effective than single modality treatments.
Ultimately, the best treatment methods and choices are determined by an experienced Neurosurgeon based on all the available information and presented to the patient for his or her final decision.
Post-Treatment Testing and Follow-Up
Some of the tests that were done to diagnose the cancer or to find out the stage of the cancer may be repeated. Some tests will be repeated in order to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back). These tests are sometimes called follow-up tests or check-ups.
The most common follow-up tests are:
A hormonal screen
Visual fields
A fundal eye exam and photo
MRI of the brain with a focus on the pituitary gland and its surroundings
Conclusion
Pituitary tumours, while often benign, can significantly impact health due to their effects on hormones and nearby structures. Early detection and treatment are essential to prevent complications and improve quality of life. If you or your loved one are experiencing symptoms related to pituitary tumours, consult a healthcare professional promptly. For expert care and personalised treatment, visit the Singapore Brain Spine Nerves Center today.
References and Acknowledgements
National Institutes of Health\ National Cancer Institute – USA
Singapore Brain Spine Nerves Center Treatment information



